
Dr. Aruna Ashok MBBS, MS OG, DNB OG
- Clinical Director
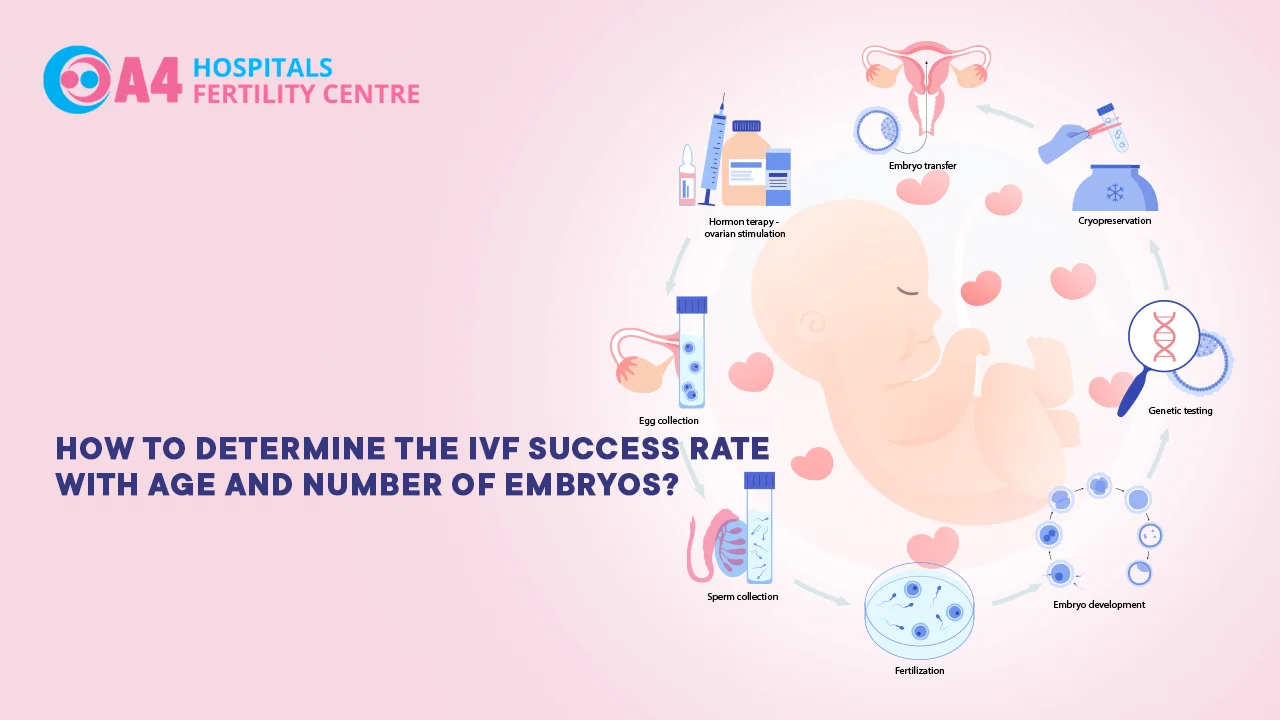
In vitro fertilization (IVF) has revolutionized fertility treatments, offering hope to couples struggling with infertility. However, the success of IVF can be influenced by various factors, with age and the number of embryos transferred playing pivotal roles.
Understanding how these factors impact IVF outcomes is crucial for patients and healthcare providers alike. In this comprehensive article, we will explore the relationship between age, number of embryos, and IVF success rates.
By delving into the intricacies of this topic, individuals can make informed decisions and fertility specialists can provide tailored treatment plans to maximize the chances of a successful IVF outcome.
Examining this relationship is like looking at a puzzle. All of the pieces must fit together to form a complete picture and without all of the pieces in place, the picture is incomplete.
In the same way, by understanding all of the factors that impact IVF outcomes, individuals and healthcare providers can come up with a comprehensive plan that ensures the best possible outcome.
As women age, their fertility declines due to a decrease in the quantity and quality of their eggs. Advanced maternal age, typically considered over 35 years, is associated with reduced IVF success rates. This decline is primarily attributed to a higher incidence of chromosomal abnormalities in older eggs, which can lead to implantation failure or miscarriage.
Prior to undergoing IVF, women may undergo ovarian reserve testing to assess their fertility potential. Tests such as measuring anti-Mullerian hormone (AMH) levels and conducting antral follicle count (AFC) can provide valuable information about ovarian reserve and help estimate the likelihood of IVF success based on age.
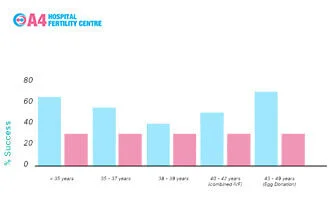
The practice of single embryo transfer (SET) has gained prominence in recent years. By transferring only one embryo, the risk of multiple pregnancies, which carry potential health risks for both the mother and the babies, is significantly reduced. SET is particularly recommended for younger patients with good embryo quality, as it can maintain high success rates while minimizing the risk of complications. The SET procedure has a high success rate, particularly for younger patients with good embryo quality. But don't worry, it's still possible to have twins with SET - just add a little extra love!
In certain cases, multiple embryo transfer may be considered, especially in older patients or those with a history of failed IVF attempts. This approach aims to increase the chances of successful implantation by transferring more embryos. However, it also escalates the risk of multiple pregnancies, which necessitates careful consideration and counseling. The success rate for a double embryo transfer with one top quality embryo and one poor quality embryo was found to be similar to a single embryo transfer with a top quality embryo.
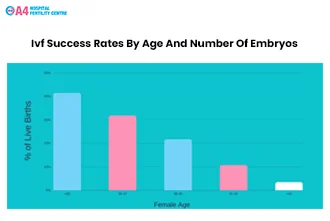
Age is a critical determinant of IVF success rates. Women under 35 generally have higher success rates compared to older age groups. As women approach their late 30s and early 40s, the decline in fertility becomes more pronounced, resulting in decreased implantation and pregnancy rates. Advanced age also increases the risk of miscarriage and genetic abnormalities in the offspring.
The number of embryos transferred significantly affects IVF success rates. While transferring more embryos may enhance the likelihood of pregnancy, it also increases the risk of multiple pregnancies and associated complications. Striking the right balance between maximizing success rates and minimizing risks is crucial, and this decision should be tailored to individual patient characteristics. So, basically, don't put all your eggs in one basket!
Prior to embarking on an IVF journey, comprehensive counseling sessions with fertility specialists are essential. These sessions provide an opportunity to discuss the impact of age, number of embryos, and other relevant factors on the success rates. Understanding the potential risks and benefits allows patients to make informed decisions and set realistic expectations. The success rate of IVF is affected by the number of embryos, number of injected oocytes, cause of infertility, female age, and PCOS.
Fertility specialists develop personalized treatment plans, considering factors such as age, ovarian reserve, and previous IVF outcomes. By tailoring the stimulation protocol, embryo selection, and transfer strategies to the unique needs of each patient, the chances of a successful IVF outcome can be optimized. The success rate of IVF is 31% in women younger than 35 years of age. 24% in women aged 35 to 37. 16% in women aged 38 to 40. 8% in women aged 41 to 44.
Determining the success rate of IVF involves considering crucial factors such as age and the number of embryos transferred. Advanced maternal age is associated with declining fertility and decreased IVF success rates. Single embryo transfer offers a safer option for younger patients, while multiple embryo transfer may be considered in specific cases. The success rates of IVF can be optimized through pre-IVF counseling and personalized treatment plans that consider individual characteristics and preferences. By understanding the intricate interplay between age, embryo number, and IVF outcomes, individuals can embark on their IVF journey with confidence, supported by evidence-based information and expert guidance.